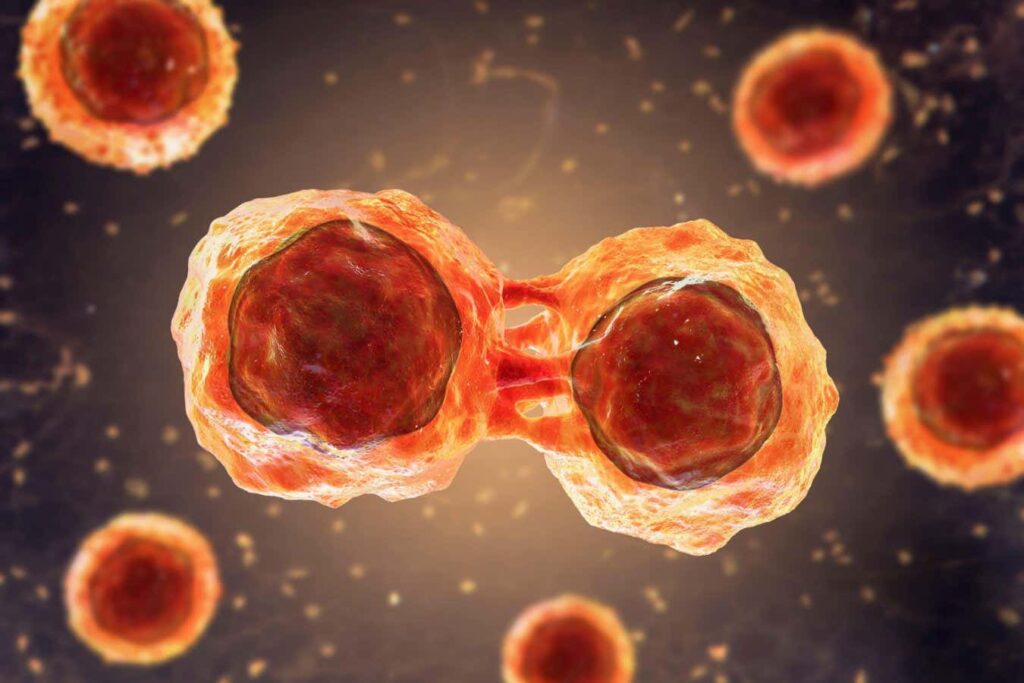
Stem cells are produced in the bone marrow and develop into different types of blood cells.
Katerina Conn / SPL/ Alamy
Human blood stem cells have been grown in a laboratory for the first time, which could dramatically improve how certain types of cancer are treated.
The lab-grown cells have so far only been tested in mice, but when injected into the animals, they resulted in functional bone marrow similar to levels seen after umbilical cord blood cell transplants.
Treating cancers such as leukemia and lymphoma with radiation and chemotherapy can destroy blood-forming cells in the bone marrow. A stem cell transplant means new healthy bone marrow and blood cells can grow. The umbilical cord is a particularly rich source of stem cells, but there is a limited amount they can provide, and the transplant may be rejected by the body.
The new method allows researchers to create stem cells from actual patients, eliminating supply issues and reducing the risk that the patient's body will reject the stem cells.
First, they transformed human blood and skin cells into so-called pluripotent stem cells through a process called reprogramming. “This involves temporarily switching on four genes, so that the patient's cells revert to an earlier stage of development that can become any cell in the body,” he said. Andrew Elefanti At the Murdoch Children's Research Institute in Melbourne.
The second step is to turn the pluripotent cells into blood stem cells. “You start by making thousands of tiny, free-floating balls of cells, each containing a few hundred cells, and then you induce them to turn from stem cells to blood vessels to blood cells,” Elefanti says. This process, called differentiation, takes about two weeks and produces millions of blood cells, he says.
When these cells were then injected into mice that lack immune systems, they produced functional bone marrow in up to 50 percent of cases. That means they made the same cells that carry oxygen and fight infection as healthy human bone marrow, Elefanti says. “This unique ability to make all blood cell types over an extended period of time defines them as blood stem cells,” he says.
Abbas Shafi A researcher from the University of Queensland in Brisbane said the work was an “exciting step forward” towards new treatments for blood cancers. “It's never been done before and has great potential for the future.” But even once animal testing is complete, he said a lot of human research still needs to be done before the technique can be used in the clinic.
Simon Cohn Researchers at Flinders University in Adelaide, Australia, say a key advantage of their approach is that it can be scaled up to produce “an essentially limitless supply” of blood stem cells, but they add that the work is based on blood or skin cells, and success rates and blood cell diversity depend on the starting cell type.
“This suggests that treatments are inconsistent even at the preclinical stage in mice, and will need to be addressed before clinical trials in human patients,” he says.
topic:
Source: www.newscientist.com