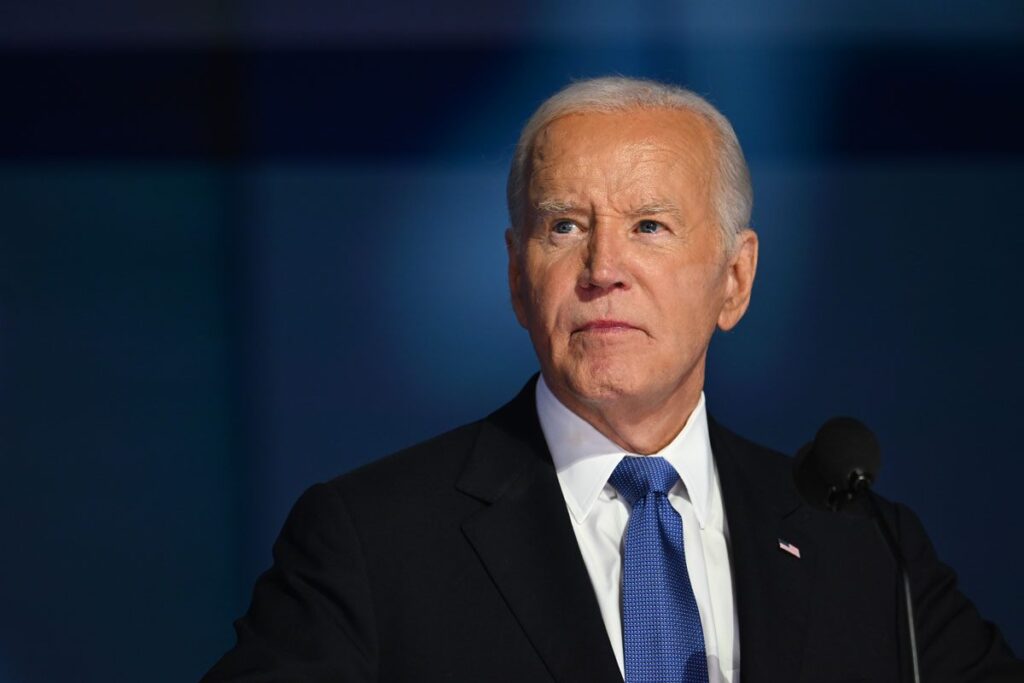
Joe Biden’s recent prostate cancer diagnosis has brought awareness to these health issues within the public discourse.
Prostate cancer charities are urging men across the country to assess their cancer risk through signs and to seek medical advice if they experience symptoms like frequent and uncontrollable urination. Nevertheless, prostate cancer remains a nuanced and intricate condition.
The prostate gland is located beneath the bladder and typically enlarges with age. The urethra, which drains urine from the bladder, passes through the prostate. Consequently, when the prostate enlarges, it can compress the urethra, impeding urine flow and leading to symptoms such as dribbling and increased urgency to urinate. Overall, this is a prevalent condition.
Likewise, the incidence of cancers originating in the prostate is quite common. Autopsy studies indicate that 36% of white individuals and 51% of African Americans had unreported prostate cancer. In the 1970s, he was diagnosed with prostate cancer.
Another study suggested that five percent of men under 30 lived with prostate cancer. This may seem surprising, but these cancers were identified during autopsies of men who passed away from other causes. Medical professionals have long maintained certain sayings, such as “That’s how I die from prostate cancer.”
This presents a significant challenge concerning prostate cancer. It can manifest in a form that causes minimal harm while also possessing a variant that is potentially lethal and can metastasize to nearby organs and bones.
How Dangerous Is Prostate Cancer?
Currently, prostate cancer accounts for approximately 35,000 deaths in the U.S. each year, with over 313,000 men diagnosed annually.
The key to addressing this issue lies in identifying which cases pose a threat, as treatments like surgery, radiation therapy, and hormone therapy may have side effects such as long-term erectile dysfunction and incontinence.
It is essential that patients avoid unnecessary treatments that do not benefit them.
Unfortunately, there is currently no straightforward method to differentiate between aggressive tumors and those that are indolent. A blood test known as the PSA (prostate-specific antigen) test was created in the 1990s to monitor men’s responses to prostate cancer treatments.
Following its introduction, the number of diagnosed prostate cancer cases surged, yet there was no corresponding decrease in mortality rates.
This led Richard Alvin, the researcher who developed the PSA test, to remark, “The widespread use has resulted in a costly public health crisis.” This is due to the PSA test potentially generating false positives caused by factors aside from prostate cancer, including infections and benign prostate enlargement.
In the U.S., the Preventive Services Task Force reviews research independently and issues recommendations regarding screening.
They state that PSA screening can marginally lower the risk of death from prostate cancer in some men. However, many men may experience harm from the screening, including false positives leading to unnecessary tests and diagnoses of non-threatening issues.
In short, increased screening rates in the U.S. may have contributed to deteriorating health outcomes for men, as they pursued treatments for conditions detected through positive test results that were not life-threatening.
Despite a reduction in testing rates since their peak in the ’90s, prostate cancer mortality rates in the U.S. have gradually decreased over the years. This might be attributed to improved treatment protocols, rather than indicating benign prostate enlargement. Limiting trials to men who exhibit symptoms of prostate enlargement could prevent unnecessary cancer treatments.
In other regions, such as in Sweden, prostate cancer screening cut mortality rates from 1.7% to 0.98%, although this required diagnosing 13 men to prevent a single death.
What is the Solution?
To mitigate this issue and avoid unnecessary treatments, a “watchful waiting” approach has shown efficacy. A recent 15-year British study indicated that localized prostate cancer with low mortality rates whether treatment included radiation, prostate removal, hormone therapy, or observation. This underscores the futility of invasive treatments offering no significant benefits.
So, what steps can we take? In the UK, the National Screening Committee regularly reviews the recommendation for PSA screening for prostate cancer. Recent research has identified harmful cancers through MRI screenings, but there is still insufficient evidence regarding whether this can reduce death rates while minimizing excessive treatments.
Meanwhile, straightforward messages regarding the benefits of screening are being communicated to men without adequately addressing the potential drawbacks. Numerous screening events are organized by well-meaning charities during sports events. Advocates argue that informed consent is critical; otherwise, we risk offering false promises and ensuring minimal progress in men’s health.
This article was published in 2024
Read more:
Source: www.sciencefocus.com