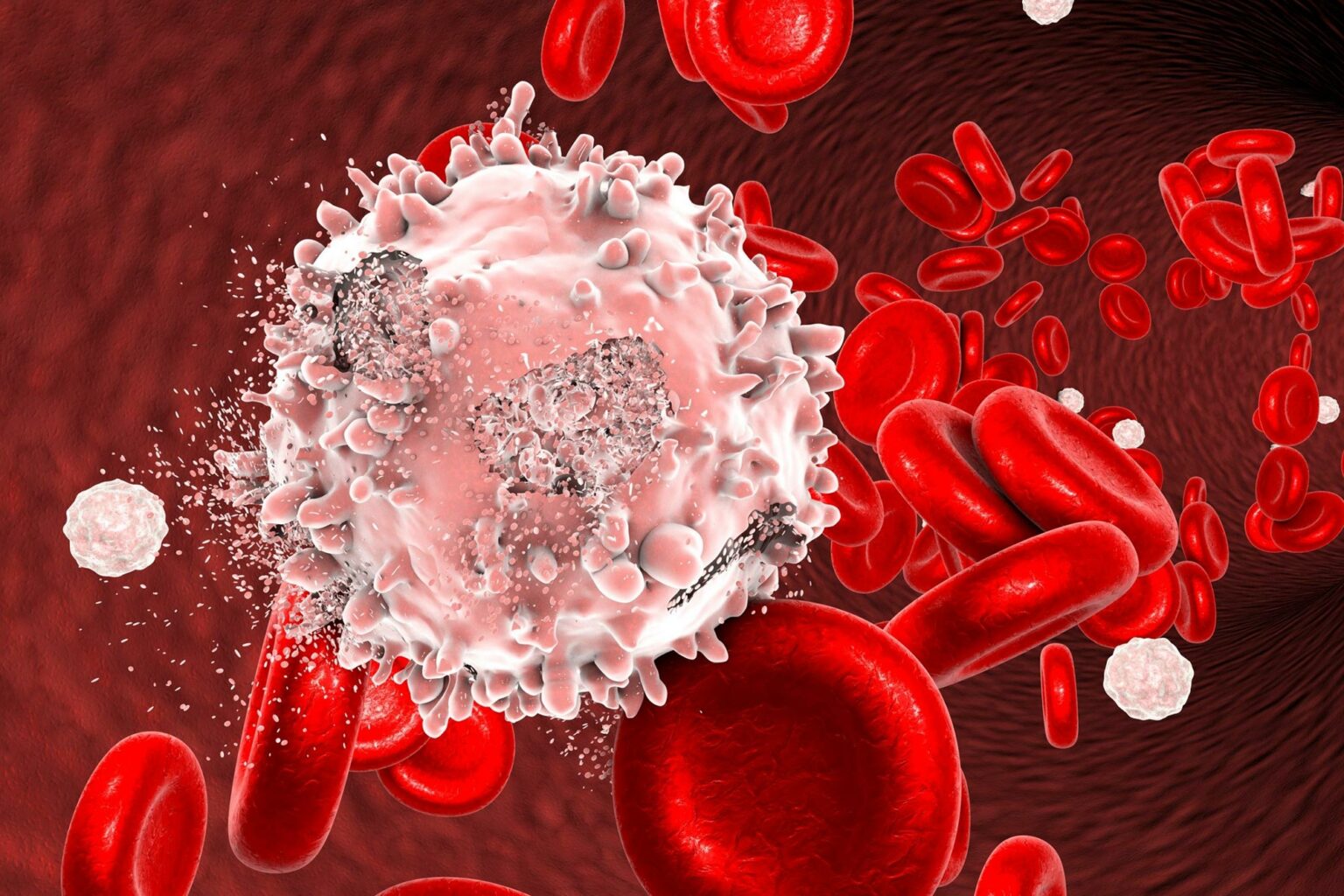
A breakthrough assay to detect acute myeloid leukemia (AML) through a KMT2A gene fusion promises to enhance diagnosis and treatment and represents a major advance in leukemia research.
The researchers Accuracy
Detecting specific molecular markers within leukemia cells has the potential to significantly improve the assessment of measurable residual disease. This advancement will enable better-informed treatment decisions and ultimately improve patient outcomes.
A new assay that detects unique molecular markers in patients with acute myeloid leukemia (AML) could revolutionize how the disease is detected and treated, according to a recently published new report. Molecular Diagnostic Journal Published by Elsevier. This assay may improve the detection of AML due to factors such as: Kuomintang 2A Gene fusions can impact treatment decision-making, assessment of response to treatment, and long-term monitoring.
AML is a rare, aggressive blood cancer that is diagnosed in approximately 120,000 people worldwide each year. Detecting residual disease during treatment is essential to determine prognosis and guide treatment decisions.Currently, methods to detect measurable residual disease (MRD) during treatment of AML include bone marrow morphology, multiparameter flow cytometry (MPFC), and DNA Sequencing.
Morphological evaluation detects leukemic cells only with a detection limit of 5%. Although MPFC has a more sensitive detection limit of 0.01% to 0.001%, it is difficult to implement and interpret and is not standardized across laboratories. DNA sequencing approaches can identify leukemic cells by somatic mutation profiles, but are expensive and can be confounded by clonal hematopoiesis in nonleukemic blood cells.
Breakthrough progress in leukemia research
“We’ve seen a lot of research in this field,” explained lead researcher Dr. Grant A. Challen, of the Department of Oncology at Washington University School of Medicine in St. Louis. Normally absent in healthy cells. Other diseases such as chronic myeloid leukemia (CML) can already be tracked by standard BCR-ABL fusions, and sensitive detection of these fusions has revolutionized the way CML is treated. . For AML patients whose disease is caused by oncogenic fusions, the KMT2A fusion is a molecular marker that can be exploited for sensitive MRD detection. Therefore, we wanted to develop a platform for sensitive KMT2A fusion detection to improve detection and treatment methods for this disease. ”
Researchers have developed a new droplet digital PCR assay that allows for high sensitivity. Kuomintang 2A Fusion detection with the five most common fusion partners.At least 80 are known Kuomintang 2A There are fusion partners, but approximately 80% of fusions involve only 5 partners – AF9, AF6, AF4, Elleand English. They benchmarked the assay in human cell lines and patient samples and demonstrated sensitivity and specificity. Kuomintang 2A Fusion detection.
This assay detects these fusions by splitting cDNA molecules into microfluidic droplets and assaying them using primers and probes that generate a positive signal only when the fused transcript is present. Researchers were able to combine multiple primer/probe sets targeting different fusions into a pooled fusion detection reagent. they again, Kuomintang 2A Fusions in patient samples are known to be present Kuomintang 2A fusion.
Implications for AML treatment and future research
Dr. Challen said: This assay can be easily extended to include additional oncogenic fusions. This has potential implications for treatment decision-making and assessment of response to treatment. Knowing whether treatment is effective is critical to deciding when to escalate treatment or perform a hematopoietic stem cell transplant. ”
“This is a powerful new tool for highly sensitive KMT2A fusion detection and can be directly applied to disease detection in leukemia patients caused by these fusions. This fills a void in oncogenic fusion detection. , we offer several technical improvements. This assay is also highly scalable, and additional fusions can be easily added to the assay to expand coverage of other oncogenic fusions. We is improving blood cancer detection one drop at a time.”
Reference: “Droplet Digital PCR for Oncogenic KMT2A Fusion Detection” by Andrew L. Young, Hannah C. Davis, and Grant A. Challen, October 7, 2023. Molecular Diagnostic Journal.
DOI: 10.1016/j.jmoldx.2023.09.006
This research was funded by: National Institutes of Health and the Leukemia and Lymphoma Society.
Source: scitechdaily.com