The urgent crisis of antibiotic-resistant superbugs is being solved in groundbreaking research by the University of Massachusetts Amherst and Microbiotics. Their research focuses on disrupting the pathogen’s type 3 secretion system, providing a new approach to preventing infectious diseases. This strategy, supported by innovative luciferase-based technology, could pave the way for new drugs, improve our understanding of microbial infections, and lead to major advances in public health. Credit: SciTechDaily.com
The team is developing tests to identify new drugs that neutralize pathogens and provide substantial benefits to public health.
Antibiotic-resistant “superbugs” could overwhelm efforts to eradicate “superbugs” are an imminent public health crisis, with more than 2.8 million antibiotic-resistant infections occurring each year, according to the CDC disease is occurring. Researchers around the world are struggling to address this challenge.
Recently, a collaborative team of researchers led by the University of Massachusetts Amherst and including scientists from biopharmaceutical companies microbiologypublished in a magazine ACS infection They said they have successfully learned how to interfere with a key mechanism used by pathogens to infect host cells, called the type 3 secretion system. Additionally, the researchers report that they have developed a test to identify the next generation of drugs that target this vulnerable cellular machinery and have real benefits for public health.
A typical strategy when treating microbial infections is to attack the pathogen with antibiotics, which work by entering and killing harmful cells. This is not as easy as it sounds. New antibiotics need to be water-soluble so they can easily pass through the bloodstream, and oil-based to cross the cell membranes that are the first line of defense of pathogenic cells. Of course, water and oil don’t mix. It is difficult to design a drug that has enough of both properties to be effective.
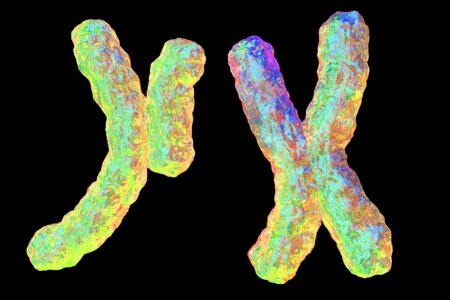
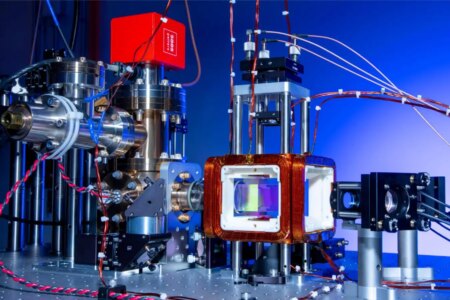
The type 3 secretion system relies on two proteins, PopB and PopD (red and blue), which form tunnels in the host cell wall.
That’s not the only problem. Antibiotics can’t cause any harm because pathogenic cells have developed something called an “efflux pump” that can recognize them and safely pump them out of the cell. If an antibiotic cannot overcome the efflux pumps and kills the cell, the pathogen will “remember” what that particular antibiotic is and create additional efflux pumps to deal with it efficiently. Develop. This means that they become resistant to that particular antibiotic.
One way forward is to find new antibiotics or combinations of them to stay one step ahead of superbugs.
“Or you could change your strategy,” says Alejandro Heuch, associate professor of biochemistry and molecular biology at the University of Massachusetts Amherst and lead author of the paper. “I am a chemist and have always been interested in understanding how chemical molecules interact with living organisms. In particular, I understand the communication between pathogens and the host cells they try to invade. We have focused our research on molecules that make this possible. If we don’t try to kill the pathogen, there’s no chance that the pathogen will develop resistance. We’re just jamming that machine. The pathogen is still alive. It’s just ineffective, and the host has no chance of developing resistance. You have time to use your natural defenses to eliminate the pathogen.”
Heuck and his colleagues are particularly interested in a communication system called the type 3 secretion system, which so far is thought to be an evolutionary adaptation unique to pathogenic microorganisms. Understanding host-pathogen interactions.
Like pathogenic cells, host cells have thick and impermeable cell walls. To overcome these, pathogens first developed syringe-like machines that secreted two proteins known as PopD and PopB. Neither PopD nor PopB can break through the cell wall on their own, but together the two proteins can create a “translocon,” the equivalent of a tunnel through the cell membrane. Once the tunnel is established, the pathogenic cell can inject other proteins that serve to infect the host. This entire process is called the type 3 secretion system, and it cannot function without both PopB and PopD. “If you don’t try to kill the pathogen, there’s no chance of it developing resistance,” Huke says. We’re just jamming that machine. The pathogen is still alive. It’s just ineffective, and the host needs time to use its natural defenses to eliminate the pathogen.
Heuck and his colleagues realized that a type of enzyme called luciferase (similar to what makes lightning bugs glow at night) could be used as a tracer. They split the enzyme into two halves. Half of it was integrated into the PopD/PopB protein and the other half was integrated into the host cell.These engineered proteins and hosts can receive a large influx of different compounds. If the host cell suddenly glows, it means that PopD/PopB has broken through the cell wall and recombined her two halves of luciferase, causing it to glow. But what if the cells remain dark? “Then we can see which molecules disrupt the translocon,” Huke says.
Huke was quick to point out that his team’s research not only has obvious applications in the pharmaceutical and public health worlds, but also advances our understanding of exactly how microbes infect healthy cells. “We wanted to study how pathogens work, and suddenly we realized that our discoveries could help solve public health problems,” he said.
Reference: “Cell-based assay to determine translocon assembly of the type 3 secretion system in Pseudomonas aeruginosa using split luciferase” by Hanling Guo, Emily J. Geddes, Timothy J. Opperman and Alejandro P. Heuck , November 18, 2023 ACS infection.DOI: 10.1021/acsinfecdis.3c00482
This research was supported by the Massachusetts Amherst Applied Life Sciences Institute, a Healey Foundation grant, and National Institutes of Health.
Source: scitechdaily.com