Measuring body fat more carefully may help treat obesity
Half Point/Getty Images
Rethinking how obesity is defined could help millions of people around the world, claims a team of researchers who want to introduce a new category of “preclinical” obesity.
The current definition of obesity as set by the World Health Organization (WHO) is having excess body fat that poses a risk to health. The WHO recommends that health professionals assess whether people are obese by calculating their body mass index (BMI), a measure of weight in relation to height. A BMI between 18.5 and 24.9 is considered healthy, while anything below or above that indicates being under or overweight. A BMI of more than 30 indicates obesity.
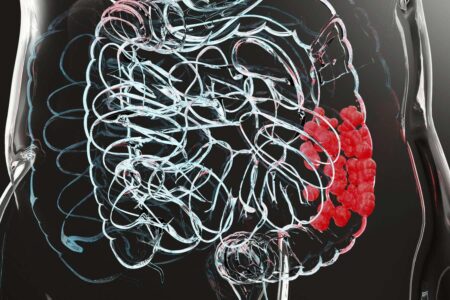
It’s true that having a lot of body fat can cause fat to infiltrate organs such as the liver and pancreas. impair function. It can also worsen inflammation and increase the risk of diseases such as cancer, liver disease, and heart disease.
However, BMI does not reflect a person’s body fat level very well. “BMI does not tell you whether that ‘excess’ weight is due to excess body fat or increased muscle and bone mass,” he says. Francesco Rubino He led research on obesity at King’s College, London.
Body fat levels, even when properly assessed by waist measurements or, in rare cases, X-ray scans, do not completely determine a person’s health status. “No two people react the same way to excess body fat. This is influenced by a person’s race/ethnicity, age, and the food they eat, with genetics playing a huge role.” says. stephen heimsfield at Louisiana State University.
That’s why Rubino and his colleagues want to introduce more nuance to the definition of obesity, separating cases into preclinical and clinical cases. Although both forms are characterized by excess body fat, only the clinical form is associated with symptoms caused by excess fat, such as difficulty breathing, heart problems, and difficulty with daily activities. Preclinical obesity, on the other hand, increases the risk of eventually developing such obesity-related symptoms, Rubino says.
This is similar to prediabetes, where blood sugar levels are higher than normal but not high enough to be diagnosed as full-blown type 2 diabetes, Rubino said.
Under the proposed changes, medical staff would use waist width and X-rays in addition to BMI calculations to directly measure people’s body fat levels, but people with a BMI over 40 would always be overweight. It will be considered fatty. Blood tests are then used to assess organ health and people are asked if they have symptoms. Blood tests are routinely done by many clinicians anyway, but directly measuring body fat would add some workload, Heimsfield says.
If the new definition is widely adopted by clinicians, it could mean people will receive more personalized advice and treatment, Rubino said. In general, people with pre-clinical obesity may only need to monitor their health and make lifestyle changes, while those with clinical obesity are more likely to need treatment with drugs or surgery, Rubino said. say.
“This allows us to better triage people and get them the right care,” he says. Adrian Brown At University College London.
Laura Gray Researchers at the University of Sheffield in the UK also welcomed the proposed changes. “It’s very necessary. These guidelines put what current research says into clinical practice,” she says. “Not all people who are obese according to their BMI are unhealthy, and not all people with a low BMI are healthy.”
This updated definition has already been endorsed by 76 health organizations around the world and may also help reduce the stigma surrounding the condition. “The hope is that by defining obesity in a more nuanced way, we will be able to show that it is a disease in itself. It is not just the result of behavior, but there are many risk factors, including environmental, psychological, and genetic. ” says Gray.
topic:
Source: www.newscientist.com