When her school closed in March 2020, Baltimore English teacher Chimere Sweeney thought that once the US got the new SARS-COV-2 virus, she would return to her students. But “There was another plan in life,” she said when she quickly got Covid and never recovered.
Initially, Sweeney developed only muscle pain. By the second week she began having panic attacks, blurry vision, constipation and partial hearing loss. Half of her face freezes “like concrete.” She forgot her phone number and address and stuttered. Within a month of contracting, she lost 30 pounds.
“In two weeks, I was told I would be better,” said Sweeney, now 42. “But my two weeks didn't come.”
Almost five years later, she still suffers from severe whole body pain, insomnia, depression, painful rash and boiling, uncontrollable urination, short-term memory loss and irregular periods.
“I'm a healthy 37-year-old woman and I might have had to pop allergy pills many times, but I took 10-12 medications per day to control almost every system in my body,” Sweeney said.
The World Health Organization characterized Covid as a pandemic on March 11, 2020, so scientists don't fully understand why some people develop chronic diseases and disordered conditions after their first virus infection. The US may have come throughout the winter after the first pandemic without a massive surge in cases, but each infection is at risk of developing a long community. Some scientists are looking for a new type of clinical trial designed for the longest and most debilitating covid patients.
Long covid is known to be the cause Over 200 different symptoms There are no approved tests or recommended treatments in almost 12 organ systems, including those of the heart, lungs, kidneys, brain, eyes and skin. Research shows long covid It's more common for middle-aged people, especially women and those with weakened immune systems, but anyone who catches the virus can get it.
The Centers for Disease Control and Prevention estimates that there is one in every 20 adults in the United States, or about 14 million. Living with a long covid. Other data shows that 5.8 million children It may be affected by the condition as well. However, experts say these numbers are likely to be underestimated as there is no official surveillance system in place.
Billion Dollar Research Initiative Called Recover Started by the National Institutes of Health, finding the causes and potential treatments of covid, I've reached that promisesays scientists and patient advocates.
Meanwhile, experts fear that extreme cuts in federal spending by the Trump administration could be possible It undermines long Covid's research effortswhich could further delay the discovery of treatment. Last month, President Donald Trump ended his secretary as a health and welfare secretary Advisory Committee on Long Covid.
W. Medical Director, UT Health Austin. Dr. Michael Broad Post-Covid-19 Program In Texas, “We build boats while we're at the sea and we're trying to understand together. [with patients] …But we need to build on the progress we have already made. ”
“We are not offering answers that are worthy of the public health crisis we are facing,” he said.
Causes of long covids
SARS-COV-2, which causes Covid, is not the only virus that causes prolonged symptoms. Another condition called myalgia encephalomyelitis/chronic fatigue syndrome (ME/CFS) shares many similarities with the long community; Caused by infection Among other things, Epstein Barr, influenza, and water cell-zoster virus.
Brode said Covid is unique because it is more likely to cause chronic disease than other pathogens. It has not yet been determined why it could lead to long-term symptoms. Experts have come to several theories so far.
One idea is that Virus remains hidden in different tissues Broad said after the infection subsided. These viral particles continue to thrust and stimulate the immune system in ways that cause long covid symptoms.
Another potential cause is Reactivation of other virusessitting in a dormant state of people's bodies, such as EBV and HIV.
Dr. Igor Coralnik, co-director of Northwest Medicine's Comprehensive COVID-19 Centre, said Covid could also trick the immune system into producing antibodies that attack people's own healthy organs and tissues.
Some evidence shows covid It affects the inner layer of blood vesselswhich leads to the formation of small clots and helps explain the symptoms, such as irregular heartbeat and heart failure, that some long-term community patients experience, Koralnik said.
It is unclear whether one or a combination of these factors will cause long covid, experts say. But the evidence suggests that they are all linked to an increase in inflammation in the body, Coralnik said, it's yours The risk of long covid increases with each covid infection.
“It's like a river that's over a dam,” Coralnik said. “The more episodes of Covid, the higher the river levels will go to where it is overflowing, and there will be a long flood of COVID symptoms.”
Diagnosis of long covids can be complicated
There are diagnostic tools to check for long covid symptoms, such as MRI scans for heart abnormalities. There are no tests that can diagnose the condition Or distinguish it from similar diseases, the CDC says.
As a result, people need to stay away from work, school or other responsibilities and endure numerous clinical tests and scans that are not only expensive, but also stressful and time-consuming. This is a broad exclusion process that prevents people from getting the help they need, Broad said.
Eye, intestine, and immune system clue
The current challenge is to find one or more biomarkers of genes, proteins, or other substances associated with a particular condition that will help diagnose long covid.
a Recover your research Released last year, routine lab tests, including 25 standard blood and urine tests, showed little difference in biomarkers, with or without previous symbiotic infections. Researchers concluded that these tests may not be useful in the diagnosis of long-term COVID.
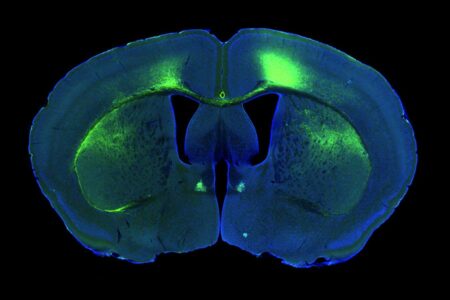
Koralnik and his team recently discovered that people with long covids are reducing blood flow in small blood vessels in the retina. This reduced flow is thought to reduce blood circulation in and around the brain, and the small organelles called mitochondria, which convert oxygen into energy, are described as “toxic.”
This theory can explain why many people with long covid experience cognitive problems, fatigue and exercise intolerance, Coralnik said. Overall, the findings published in the Journal of Imaging in February are The retina can become a long covid biomarker.
Other studies suggest that biomarkers may be present in the gut and immune system, but Brode noted that these early findings are based on small groups of people and should be considered in salt grains.
As useful as diagnostic tests, experts say that for those with prolonged symptoms, some experts should not slow scientists in searching for long covid treatments.
Julia Moore Vogel, senior program director at Scripps Research, and Patient-led research cooperation Regarding long covid, he said that other conditions like migraines do not have reliable biomarkers or tests to confirm the diagnosis. Several drugs have been approved To handle it.
“I think we'll get there,” said Vogel, a long-distance runner before developing the long-time Covid in 2020. “But I personally don't think it should contain anything.”
Unfortunate advances in long covid treatments
The Food and Drug Administration has not approved treatments, particularly for long covids. Experts are not sure if they'll get it anytime soon.
“When I first got sick, I was OK, I had to survive for just three to five years. At least, I think I have options as I have decent symptom management trial data. But we've made little progress in treatment,” Vogel said. “There are currently promising research beginning, but it's not close to the amount that should be burdened by the disease.”
Most clinical trials test whether medications used to treat other conditions are useful for long-term COVID. For example, researchers at the University of British Columbia Low-dose naltrexone – Approved drugs for opioid and alcohol use disorders. The drug is thought to have anti-inflammatory and pain relief properties and is used off-label in people with fibromyalgia and ME/CFS, making it potential as a long-term symbiotic treatment.
Other drugs Barishinibapproved for treating rheumatoid arthritis and acute charlation, and Temelimabuexperimental drugs often administered to people with multiple sclerosis have also been investigated as potential long covid treatments.
Instead of a particular treatment, people with long covids must balance rest and activity in a strategy called pacing and undergo physical and cognitive behavioral therapy for further support. Many people will often rely on several drugs, including antiviral Paxlovid, to treat symptoms.
But realistically, “we may not actually have one silver bullet treatment,” says Alison Cohen, an epidemiologist at the University of California, San Francisco, who coexisted for three years for a long time. Cohen said that long covid will take a “multi-faceted approach” to take a “multi-faceted approach” in a very diverse way.
What will you do in the future for recovery?
As long as SARS-COV-2 continues to spread, everyone is at risk of a long Covid, Cohen said. And now, evidence shows that recovery from the condition is rare. A survey released last month found it Only about 6% of people with long covid recover According to Cohen, two years later. Covid vaccinations were associated with better long-term recovery, especially among those who won booster shots.
People who improve are experiencing many “ups and downs,” Coralnik said. “You need to expect a lot of collisions on the road.”
“Living with a long Covid is tiring,” Cohen said. “So for everyone who doesn't live with it, it's important to think about what we can do to support those who have them.”
In the meantime, clinical trials must be designed to accommodate and include the patients they intend, Vogel said. Many people are tied to their homes and beds and cannot travel due to the risk of multiple in-person visits or flare-ups of symptoms, she added. “There are too many things you can't know until you put them on the table,” she said.
Although we don't know when a long community community finally gets the answers and security they need, Vogel keeps her head high.
“We know we can do that. We are confident that a well-designed and well-tested exam will at least improve the quality of life. “But I can't think of any other way. I can't accept that this is for my life.”
Source: www.nbcnews.com