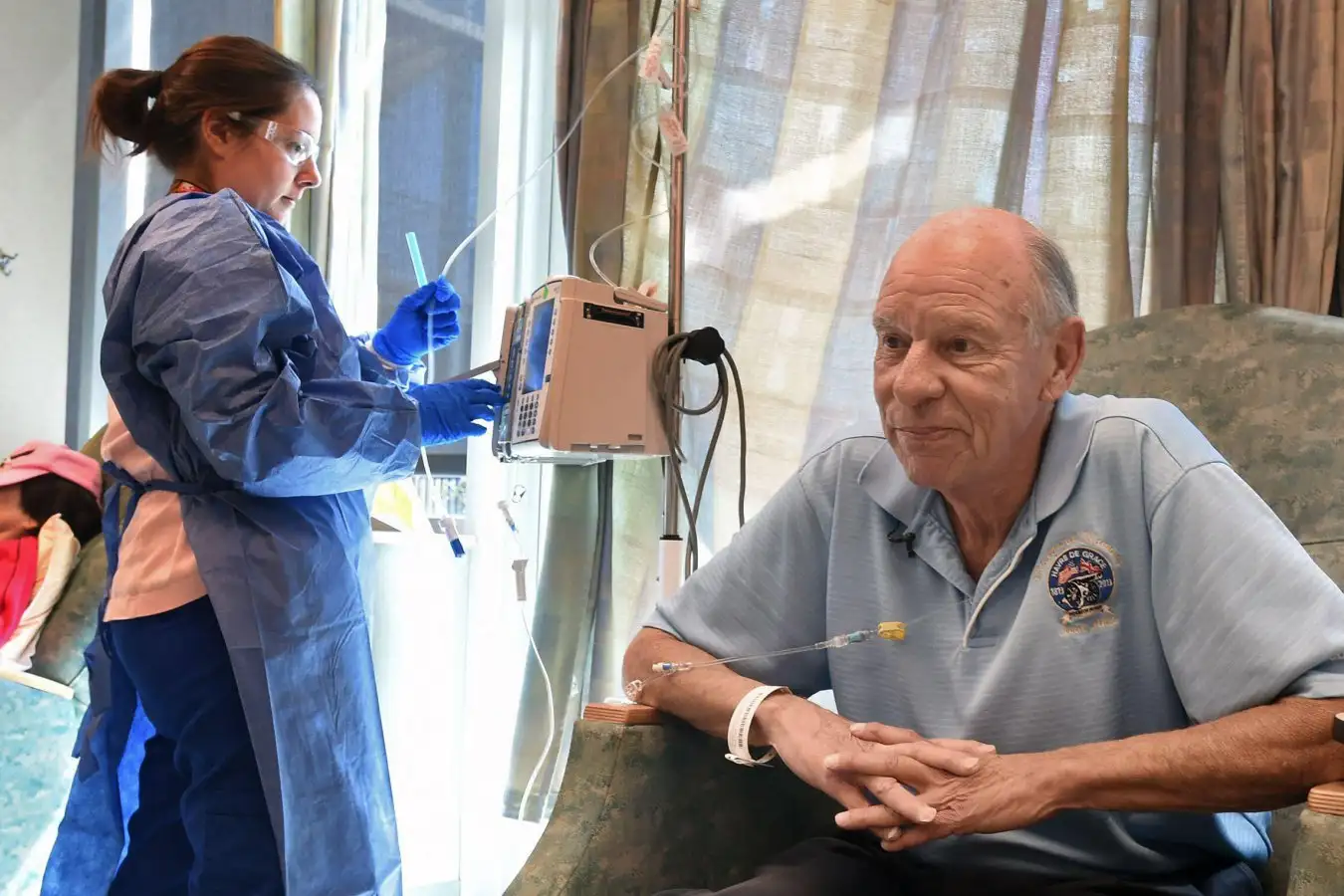
Deep brain stimulation is already utilized for Parkinson’s disease
Living Art Enterprise/Science Photo Library
Brain implants capable of detecting pain and responding with deep brain stimulation may provide relief for individuals suffering from previously untreated chronic pain.
Chronic pain affects approximately 20% of the population in the United States, and many find little relief through traditional pain management approaches. This could be due to underlying changes in brain circuitry.
Deep brain stimulation (DBS) involves using tiny electrodes to stimulate the brain, showing potential but also yielding inconsistent outcomes. The conventional method has typically applied a one-size-fits-all targeting of brain regions, despite indications that pain can stem from varying circuits in different individuals.
Thus, Prasad Shirvalkar and his team at the University of California, San Francisco, explored whether a personalized system might yield better results. In their study, six individuals with previously untreated chronic pain had their intracranial brain activity recorded and stimulated across 14 locations in the brain for ten days.
Out of five participants, the researchers pinpointed specific sites and stimulus frequencies that resulted in the most significant pain relief. While one participant noted no substantial relief, he could hold his wife for the first time in years, a notable improvement in his physical capabilities.
The research team employed machine learning to analyze and differentiate the electrical patterns associated with high and low pain levels. Consequently, they implanted permanent DBS electrodes personalized for each participant to monitor brain activity and optimize stimulation for pain detection and deactivation during sleep.
After six months of adjustments, each device underwent a trial where participants experienced real personalized stimulation for three months, followed by fake stimulation for another three months, or vice versa. The false stimulation targeted non-ideal locations with very low frequencies, and pain metrics were monitored multiple times daily throughout the trial.
On average, authentic stimulation led to a 50% reduction in daily pain intensity compared to the increase observed with spurious stimulation. Notably, the daily step counts increased by 18% during the false stimulation phase. Participants also reported fewer depressive symptoms and less pain interfering with daily life when undergoing real stimulation. These improvements persisted for over 3.5 years post-trial.
“This significant study employs the latest tools,” remarks Tim Dennison from Oxford University.
A previous challenge with DBS technology involved habituation; the brain would adapt to continuous stimulation, diminishing its effectiveness. Dennison suggests that extended benefits may arise from stimulating participants only when pain levels are elevated. The next phase will involve comparing adaptive versus constant stimuli to evaluate differences in outcomes.
“The other major hurdle lies in the economic feasibility and scalability of this method,” Dennison notes.
Topic:
Source: www.newscientist.com