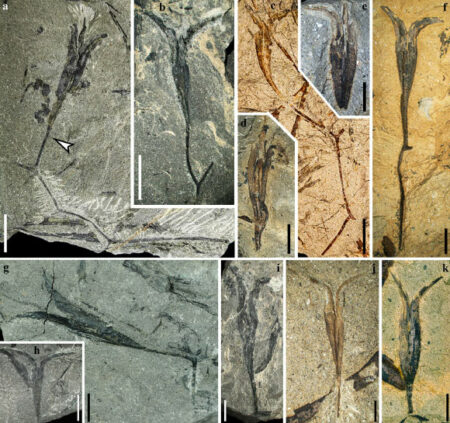
A ball of cells grown from amniotic fluid. Red indicates lung stem cells
Giuseppe Cara, Paolo di Coppi, Mattia Guerli
Babies born with serious medical conditions may one day receive better diagnosis and treatment in utero, thanks to a new technique that takes samples of cells from intrauterine fluid and grows them in dishes. It might become.
world's first, paolo de coppi Researchers at Great Ormond Street Hospital in London have shown that fetal cells from amniotic fluid can be induced to form miniature spheres of lung, kidney or small intestine tissue. They also showed that these lung organoids could help treat babies born with a sometimes fatal lung disease called congenital diaphragmatic hernia (CDH).
Although the technique has not yet been used to treat children, the results show it is possible in principle, De Coppi said. The strategy, which researchers call “personalized prenatal medicine,” can also be modified to help treat a variety of other congenital conditions.
The idea takes advantage of a recent approach in which cells in a dish are induced to grow into lentil-sized tissue organoids that take on a three-dimensional structure. These are better than standard techniques of growing cells in two-dimensional layers to capture specific aspects of the tissue in question, such as whether the tissue is healthy or growing abnormally.
The researchers now show that samples of amniotic fluid taken during pregnancy contain fetal cells that can form tissue organoids for the lungs, kidneys, and small intestine.
Studying organoids made from cells from fetuses known to suffer from congenital disorders can tell doctors exactly what form they take, how severe they are, and how they can be treated. We may be able to provide further information.
The researchers created organoids for 12 fetuses with CDH, which causes abdominal organs to push up into the chest, preventing the left lung from growing properly. This condition can be treated by pushing a balloon into the baby's lungs while the baby is in the womb to expand the lungs and improve growth.
The researchers created lung organoids from the fetuses before and after balloon treatment. They found hints that the organoids created after the treatment behaved more like healthy lung tissue than those created beforehand, suggesting that the treatment was successful.
Therefore, organoid technology can be used not only to monitor whether a treatment is effective, as doctors perform this intervention only in the most severe cases, but also to determine whether treatment is needed in the first place. You can use it.
“This has great potential for functional diagnostics,” says De Coppi. “We know how to make diagnoses based on images, but sometimes there are extensive diagnoses. [condition severity] Possible. We want to provide better prenatal diagnostic tools. ”
“If we can classify a disease as mild, moderate, or severe, that's a huge accomplishment,” he says. Cecilia Goeterstrom At Karolinska Institutet, Stockholm, Sweden.
holm schneider Researchers at Germany's Erlangen University Hospital say their approach suggests that organoids could one day be converted into mature tissue and transplanted into babies after birth, even if part of their intestine is missing, for example. ing. “If we could engineer gut-like structures for these children to use after birth, we would be in a much better position,” he says.
topic:
Source: www.newscientist.com