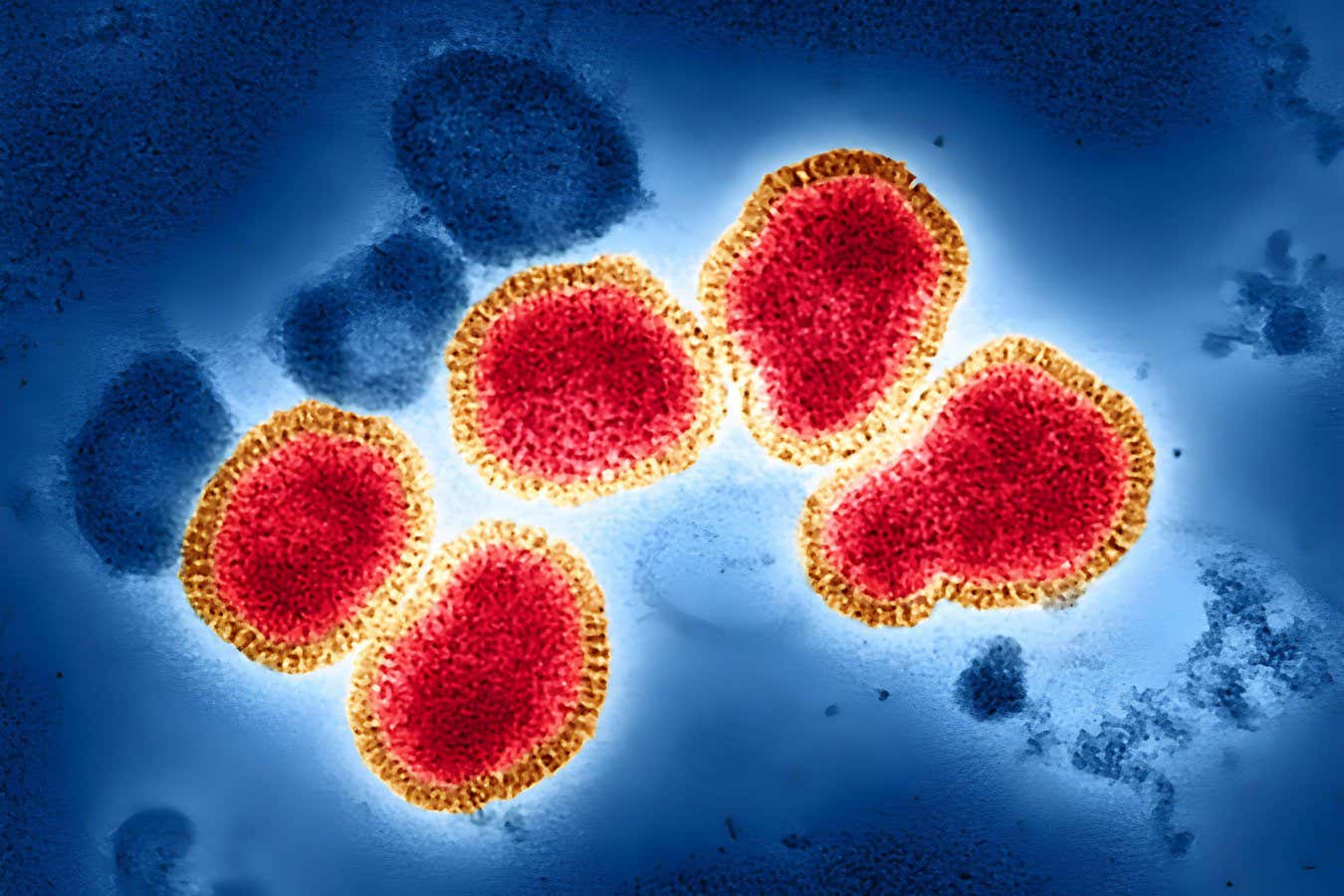
Influenza virus particles observed through an electron microscope, color enhanced
John G/Imago/Alamy
A promising long-term antiviral medication may offer protection against all strains of influenza, providing hope for the most vulnerable populations.
The flu results in the loss of thousands of lives annually, and the swift emergence of new variants poses a risk for future pandemics. Each year, scientists reformulate flu vaccines to correspond with the strains that are projected to be prevalent in the upcoming season. These vaccines prompt the immune system to generate antibodies that block the virus from infiltrating the cells.
Efforts are underway to develop a universal influenza vaccine capable of safeguarding individuals from all strains, yet these vaccines face challenges.
“Even if the first approved universal influenza vaccine is created, individuals exhibit varying immune responses, meaning not everyone will be effectively protected,” says Jeffrey Stein, CEO of Cidara. For instance, vaccines often show reduced efficacy in older adults or in those with compromised immune systems.
To tackle this issue, Stein and his team have developed a treatment known as CD388, which includes Zanamivir, an antiviral drug authorized for treating infections caused by all influenza variants that affect humans. Normally, Zanamivir is eliminated from the body within hours, but the research team has modified it to rapidly neutralize the invasive influenza virus. “It’s not part of the immune system,” Stein explains.
For testing, the team enrolled 5,000 participants aged 16-64 from the US and the UK at the beginning of the 2024 flu season. None of the participants were at elevated risk for flu-related complications or had received that year’s flu vaccine. They divided the participants into four approximately equal groups. Three groups received one injection of CD388 at low, moderate, or high doses, while the final group received a placebo.
About six months later, researchers assessed the number of individuals with symptomatic flu infections during the flu season, defined by the presence of influenza virus DNA in nasal swabs and flu-like symptoms such as cough and fever.
Thirty-three individuals in the placebo group reported symptomatic flu, whereas only eight participants in the high-dose CD388 group did, marking a risk reduction of around 76%. The moderate and low-dose groups saw a 61% and 58% decrease in risk of symptomatic infections, respectively. “All doses demonstrated significant protection against influenza illness,” states Nicole Dhabapana, Chief Medical Officer of Sidara. Side effects, such as injection site tenderness, were consistent across both the treatment and placebo groups.
The results indicate that CD388 may offer a more straightforward means of protecting individuals compared to vaccines. “[Unlike vaccines, it] does not need to match the circulating strain, and could be more effective during a ‘poor match’ year or for pandemic preparedness, especially if new flu strains, such as H5N1, transmit to humans,” remarks Pennyword from King’s College London. She adds that, based on previous data on Zanamivir, it is unlikely that influenza strains will develop resistance to it.
This approach is likely to be effective for older individuals and those known to have poor vaccination responses, including the immunocompromised. Davalpana mentions that the team plans to conduct tests on individuals aged 12 and older with compromised immune systems.
Instead of replacing vaccines, Stein suggests that the drug may work best in conjunction with them, although this has yet to be tested. Nevertheless, the findings are timely given the growing hesitance surrounding vaccinations. “We aim to bypass the controversy that unfortunately surrounds vaccines,” Stein remarks.
Topic:
Source: www.newscientist.com