Examining Resilience to Alzheimer’s Disease: Why Some Individuals Remain Symptom-Free Associated Press/Alamy
Recent studies reveal that some individuals exhibit brain changes tied to Alzheimer’s disease yet show no symptoms like memory loss. Though the reasons remain unclear, innovative research is uncovering protective factors that may prevent cognitive decline.
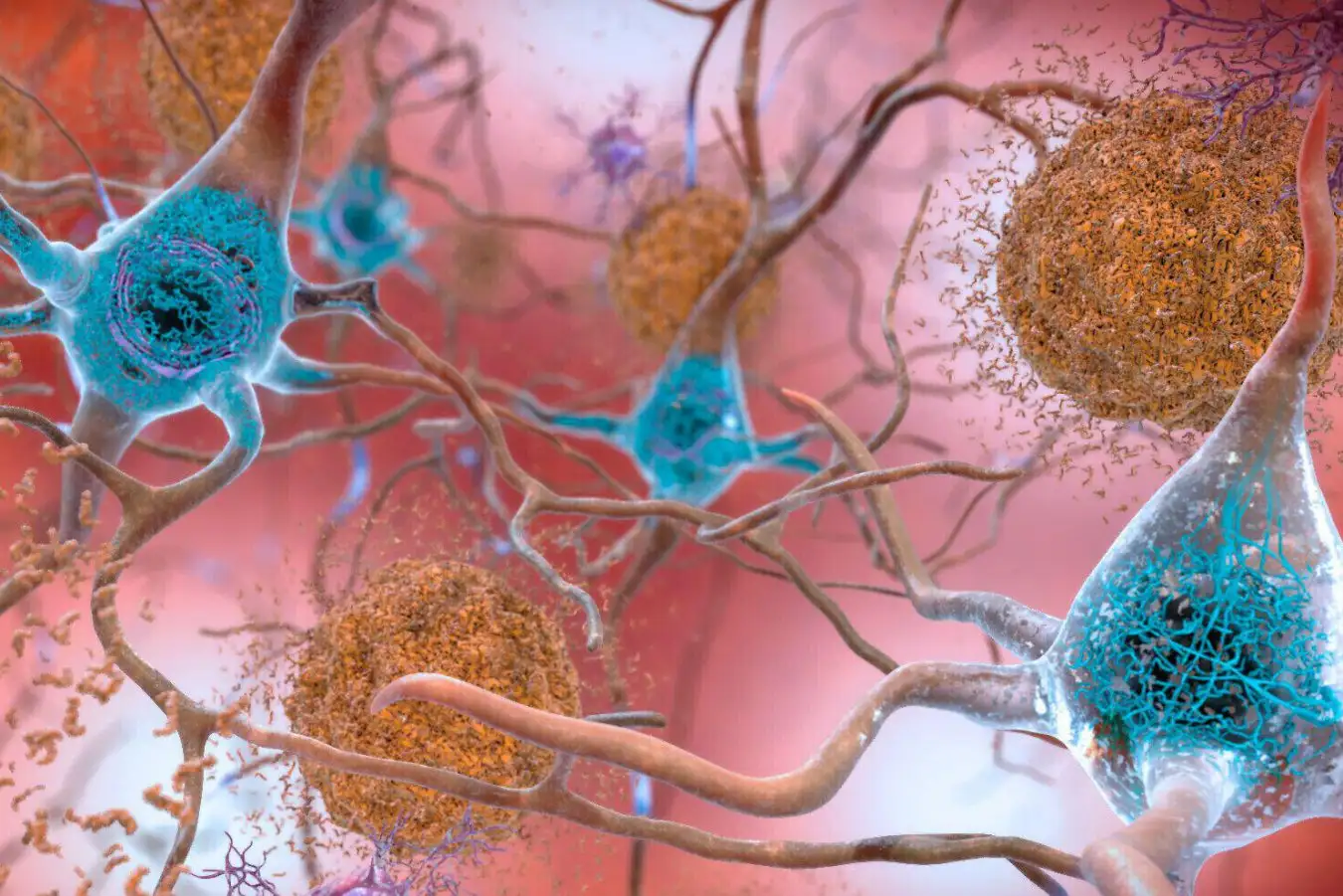
Alzheimer’s disease is marked by amyloid plaques and tau tangles accumulating in the brain, widely believed to contribute to cognitive decline. However, some individuals, known for their resilience, defy this notion. In 2022, Henne Holstege and her team at the University Medical Center in Amsterdam discovered that certain centenarians retain good cognitive function despite these pathological changes.
Expanding on this research, the team conducted a new study involving 190 deceased individuals. Among them, 88 had Alzheimer’s diagnoses, while 53 showed no signs of the disease at death. Their ages ranged from 50 to 99, and 49 were centenarians with no dementia, though 18 exhibited cognitive impairment previously.
The focus was on the middle temporal gyrus—an early site of amyloid plaques and tau tangles in Alzheimer’s. Interestingly, centenarians with elevated amyloid levels had tau levels akin to those without Alzheimer’s, suggesting that limiting tau accumulation is critical for resilience, according to Holstege.
While amyloid plaques are linked to cognitive decline, Holstege posits that tau accumulation may activate a cascade of symptoms. Notably, amyloid plaques alone may not cause significant tau tangling. “Without amyloid, tau can’t spread,” she explains.
Further analysis of approximately 3,500 brain proteins revealed only five were significantly associated with high amyloid plaques, while nearly 670 correlated with tau tangles. Many of these proteins are involved in crucial metabolic processes like cell growth and waste clearance. Holstege emphasizes, “With amyloid, everything changes; with tau, it’s a different story.”
In the cohort of 18 centenarians with high amyloid levels, 13 showed significant tau spread throughout the middle temporal gyrus, a pattern similar to Alzheimer’s, but the overall tau presence remained low.
This distinction is vital, as diagnosis hinges on tau spread, indicating that accumulation, not just proliferation, triggers cognitive decline. “We must understand that proliferation doesn’t mean abundance,” Holstege clarifies.
In a second study, Katherine Prater and her team at the University of Washington examined 33 deceased individuals—10 diagnosed with Alzheimer’s, 10 showing no signs, and 13 deemed resilient. Most subjects were over 80 and underwent cognitive assessments within a year before death.
In line with previous findings, the research indicated that tau was present but not accumulated in resilient brains. Though the mechanisms remain elusive, Prater theorizes that microglia—immune cells regulating brain inflammation—might play a crucial role in maintaining cognitive function in resilience.
Previous research has shown that microglia often become dysfunctional in Alzheimer’s disease, contributing to degenerative processes. While the researchers could not analyze microglia extensively, Holstege noted their significance.
The team also conducted genetic studies on microglia from the dorsolateral prefrontal cortex, essential for managing complex tasks. They discovered that resilient individuals’ microglia exhibited heightened activity in messenger RNA transport genes compared to those with Alzheimer’s. This suggests effective gene transport, vital for protein synthesis, is preserved in resilient brains.
“Disruptions in this process can severely impact cell function,” Dr. Prater remarked at the Neuroscience Society meeting in San Diego. However, its direct relationship to Alzheimer’s resilience remains to be elucidated.
Moreover, resilient microglia demonstrated reduced activity in metabolic energy genes compared to those in Alzheimer’s patients, mirroring patterns in healthy individuals. This suggests heightened energy expenditure in Alzheimer’s due to inflammatory states that disrupt neuronal connections and lead to cell death.
“Both studies indicate that the human brain possesses mechanisms to mitigate tau burdens,” Prater concludes. Insights gained from this research could pave the way for new interventions to delay or even prevent Alzheimer’s disease. “While we aren’t close to a cure, the biology offers hope,” she stated.
Topics:
- Brain/
- Alzheimer’s Disease
Source: www.newscientist.com