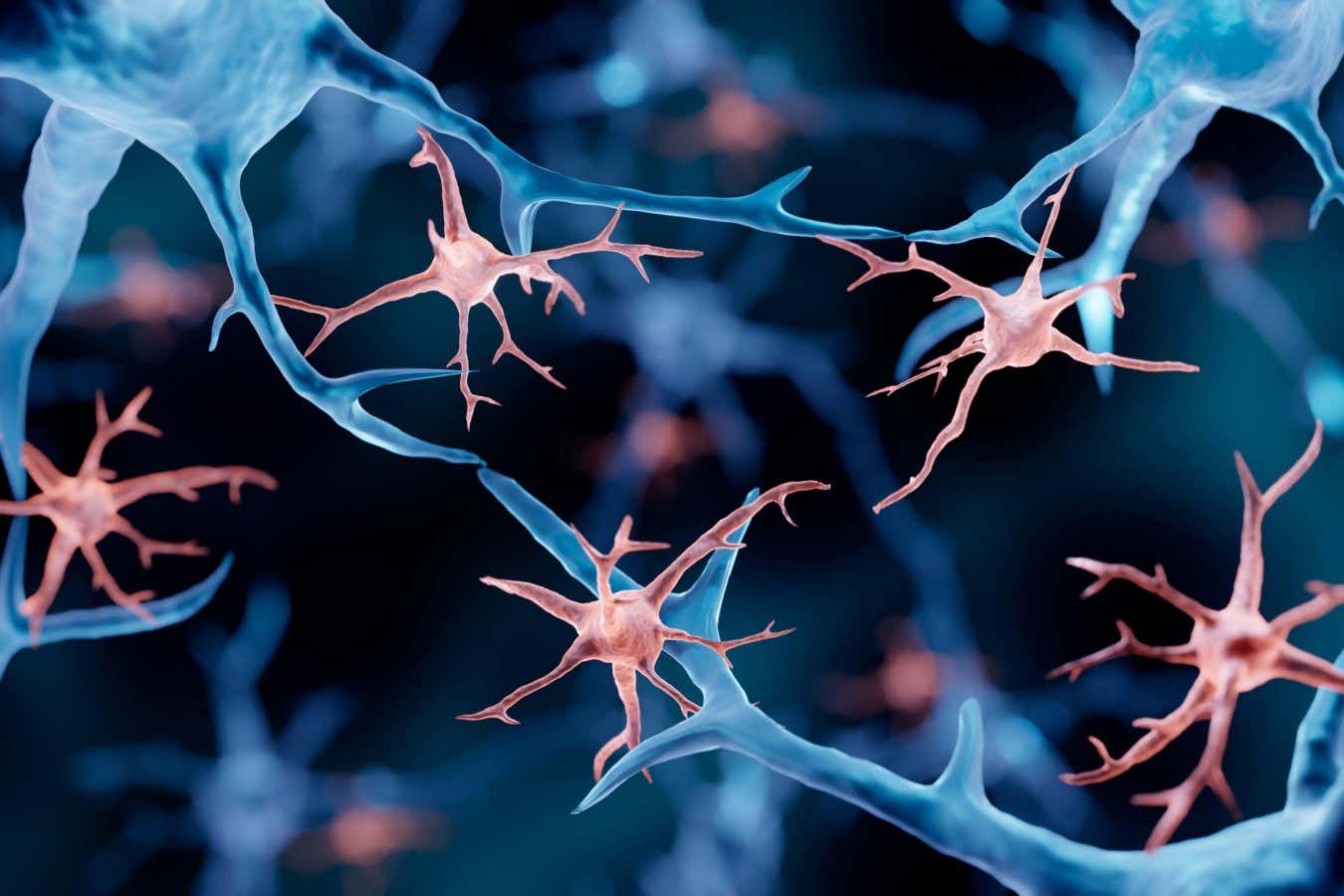
Microglia are specialized immune cells in the brain
Science Photo Library/Alamy
The process of replacing immune cells in the brain halts the advancement of a rare and terminal brain disorder known as ALSP. This also paves the way for future clinical trials targeting other neurological ailments.
Extensive research indicates that impaired microglia—specialized immune cells within the brain—play a role in various neurological disorders, including Alzheimer’s disease and schizophrenia. The term ALSP stands for adult-onset leukoencephalopathy with axonal spheroids and pigmented glia, characterized by mutations in genes responsible for the survival of these cells, resulting in a reduced number of microglia and leading to progressive cognitive decline. Currently, no effective treatment exists for this fatal illness.
To address this, Bo Peng from Fudan University in China and his team employed a novel treatment called microglia replacement therapy. Prior experiments in rodents have shown that implanted stem cells—capable of developing into different cell types—can effectively replace microglia. However, it is necessary to first eliminate existing microglia in the brain to facilitate this. This can be achieved using drugs that target protein microglia.
Pursuing this avenue, Peng and his colleagues conducted initial tests on five mice with genetic mutations analogous to those associated with ALSP. As the mutations already impacted protein microglia, the researchers did not need to deplete these proteins with medication. Subsequently, they transplanted stem cells from healthy mice into the affected mice. Fourteen months later, treated mice exhibited approximately 85% more microglia in their brains compared to six untreated mice harboring the same mutation. Notably, these treated mice also demonstrated improvements in motor function and memory.
Encouraged by these promising findings, the researchers extended the treatment to eight individuals diagnosed with ALSP, using donor stem cells without preconditions. One year post-treatment, brain scans revealed minimal changes in participants compared to scans taken before the procedure. In contrast, four untreated individuals displayed significant brain deterioration and lesions over the same period. This implies that microglial replacement therapy effectively halted the progression of the disease.
At the study’s outset, all participants underwent cognitive assessments using a 30-point scale, where a decrease in score indicated cognitive decline. Reassessments a year later showed that, on average, scores remained stable for those who received the microglia replacements.
These results point to microglial replacement therapy being a potentially effective solution for ALSP. However, since this represents the inaugural human trial, “we remain unaware of any potential side effects,” comments Peng. “Given the rapidly progressive and lethal nature of this disease, prioritizing benefits over possible side effects might be crucial.”
Chris Bennett from the University of Pennsylvania cites the historical use of stem cell transplants for treating neurological disorders. “It has demonstrated effectiveness, particularly through microglia replacement,” he states. Recent FDA approvals for two similar therapies addressing other rare brain conditions further support this. “While prior studies may not have used this exact terminology, they effectively addressed similar conditions,” Bennett elaborates. “I’d describe this as a smart and innovative application of stem cell transplants. Nonetheless, microglia replacement therapy has been evolving for decades.”
Despite this, the results underscore the broader implications of microglial replacement therapy. Experts believe this strategy could one day address more prevalent brain disorders. For example, certain genetic mutations significantly heighten Alzheimer’s disease risk and affect microglial function. Replacing these malfunctioning cells with healthy human equivalents could offer a promising avenue for treatment.
Topics:
- Neuroscience /
- Immune System
Source: www.newscientist.com